Bill Smarter.
Claim More.
RCM Automation Built for ABA's Unique Payer Challenges
- Get Paid 2x Faster
- Save 70+ Hours Monthly
- Affordable Per Client Pricing
RCM Automation Built for ABA's Unique Payer Challenges
Face Revenue Hits
from Staffing Woes
Denied Claims Are
Not Resubmitted
Annual Revenue Lost
to Inefficient Billing
Average Cost to Rework
Each Denied Claim
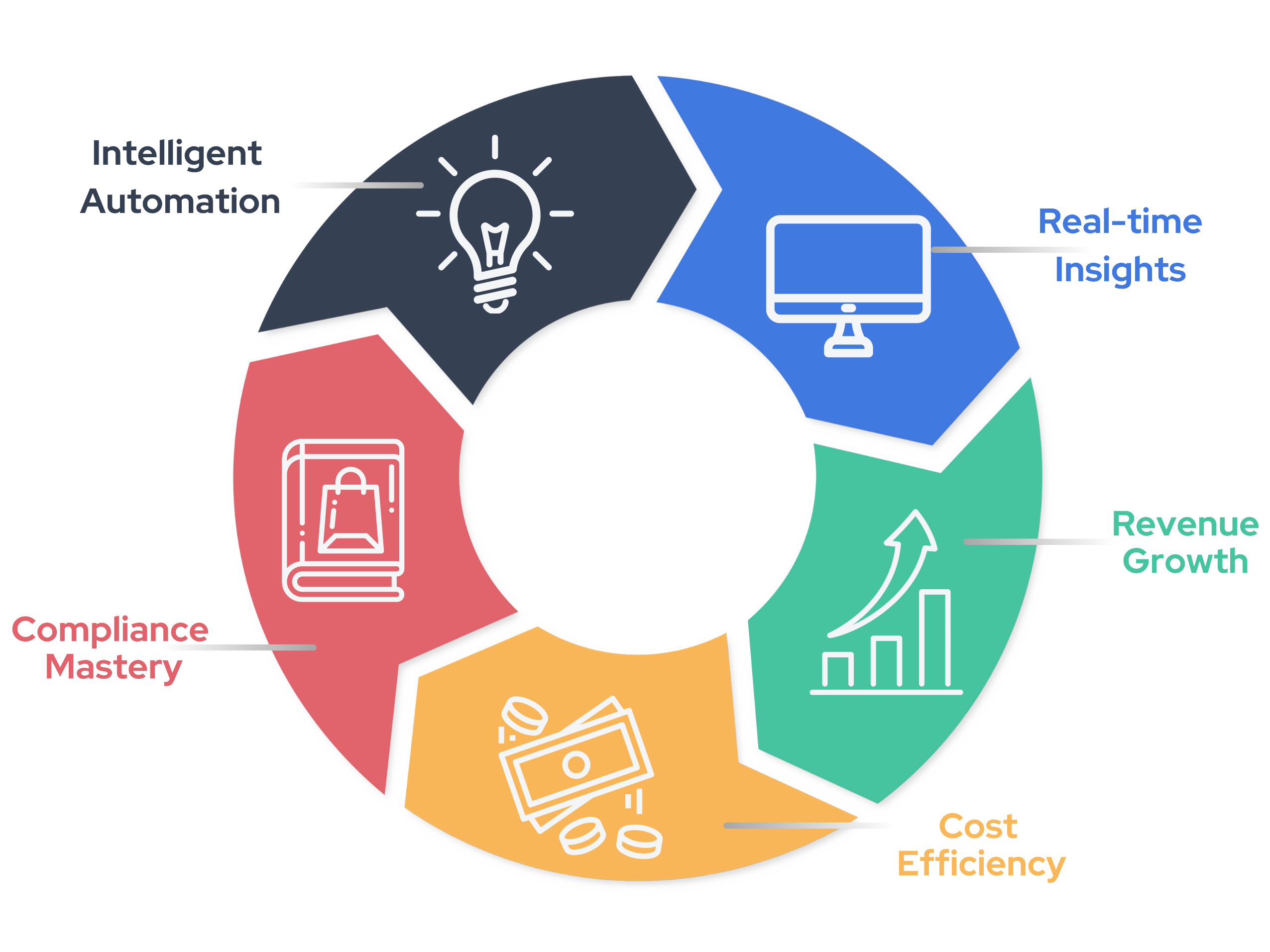
Neuromnia brings vertical integration to ABA revenue cycle management by preventing denials before they happen and automating appeals when they do. The result? More revenue, less overhead, and no disruption to your clinical workflows.
| Self-Service | RCM Vendor | Neuromnia | |
|---|---|---|---|
|
|
~$120K/year for $2.5M claims | 4-7% + admin fees ($3K-6K) | ~50% of market price |
|
|
Complete control, high manual work | Limited visibility, delayed updates | Full control with automation |
|
|
Manual appeals, 30-40% denial rate | Varies by vendor expertise | AI predictive flags, Auto-appeals |
|
|
Manual code & auth tracking | Templates + audit fees | Real-time code checks included |
|
|
60-65% | 75-80% | 90-95% |
* Calculations assume a baseline of 70 hrs/month saved at 25 clients, reducing denial rate to 5%, and typical RCM fees of 5%. Actual results may vary based on your specific situation.
Four Steps to Simplified ABA Billing
Pull session data and authorizations directly from your EHR, or upload via spreadsheet.
Catch compliance issues before claims go out, from CPT codes to expired auths.
Get clean claims out fast with automated billing and track every submission.
Stay on top of your cash flow with real-time denial tracking and appeal automation.
"We were losing $20K monthly to denied claims with our 6% biller. Within a month after signing up for Neuromnia's pilot, our denials dropped from 30% to under 5%. Not only did we save $4,800 in monthly billing fees, but their AI prevented $16K in denials our first month alone. For a small practice like ours, that's money we thought was gone forever. Now I finally get to focus on my clients instead of spending my afternoons on hold with payers."
Lauren Widerski
BCBA Owner
If you don't see an answer to your question, please send us an email.
No. If your EHR supports APIs, we sign a Business Associate Agreement (BAA) with them for HIPAA compliance and plug in directly to retrieve claims, session notes, and authorization details. If not—or if you don't have an EHR—you can simply upload a CSV file each billing cycle.
Each month, we reconcile active patients (those for whom you submit claims) and charge per patient. If a child discontinues services or you enroll someone mid‑month, our system adjusts accordingly. We keep it simple with a monthly census update, so you only pay for the patients you're actively serving.
Absolutely. Neuromnia constantly updates its database with payer‑specific rules (including TRICARE, Medicaid, and commercial carriers). For multi‑payer clinics, the AI flags each claim according to that specific payer's requirements—like correct modifiers, telehealth codes, or state‑specific guidelines.
Our system automates all possible tasks—like drafting appeals, applying updated codes, or generating supporting documents. However, direct calls or lengthy negotiations remain under your control. If the denial is more complex, you can request our case expert escalation for tailored advice or advanced appeal letters, but we do not place calls ourselves.
Yes. Our model is specifically trained on thousands of ABA claims to detect the most common denial triggers—such as missing or incorrect modifiers, expired authorizations, supervision ratio gaps, or time‑unit discrepancies. This is part of our Enhanced (proactive) tier, but the Basic tier can still auto‑appeal errors found post‑submission.
Our dashboard tracks your pre‑ and post‑Neuromnia denial rates, average turnaround times, and recovered revenue. We often see a 10–15% improvement in collection rates, translating to $3k–$6k+ monthly for a mid‑size clinic. We also save your staff from hours of manual rework, which you can track in our built‑in productivity metrics.
Neuromnia's AI monitors all remittances (835 data) in real time. If a claim is partially paid, we file an appeal or a re‑submission—depending on the payer's specific guidelines. For more complex scenarios, you can use our human case escalation to ensure thorough documentation and justification for the additional hours.
Yes, but only what's essential for processing claims and generating appeals. We are fully HIPAA‑compliant: data is encrypted at rest and in transit, we maintain strict access controls, and we never use PHI for non‑billing purposes. All training of our AI models is done with de‑identified data where possible.