Nia Chat in Action
Effortless Documentation and Insights
Problem Statement
Staff often waste 25–35% of their time on manual data entry, multiple dashboards, and duplicative paperwork—leading to inconsistent outcomes and constant frustration - a recipe to avoid for burnout.
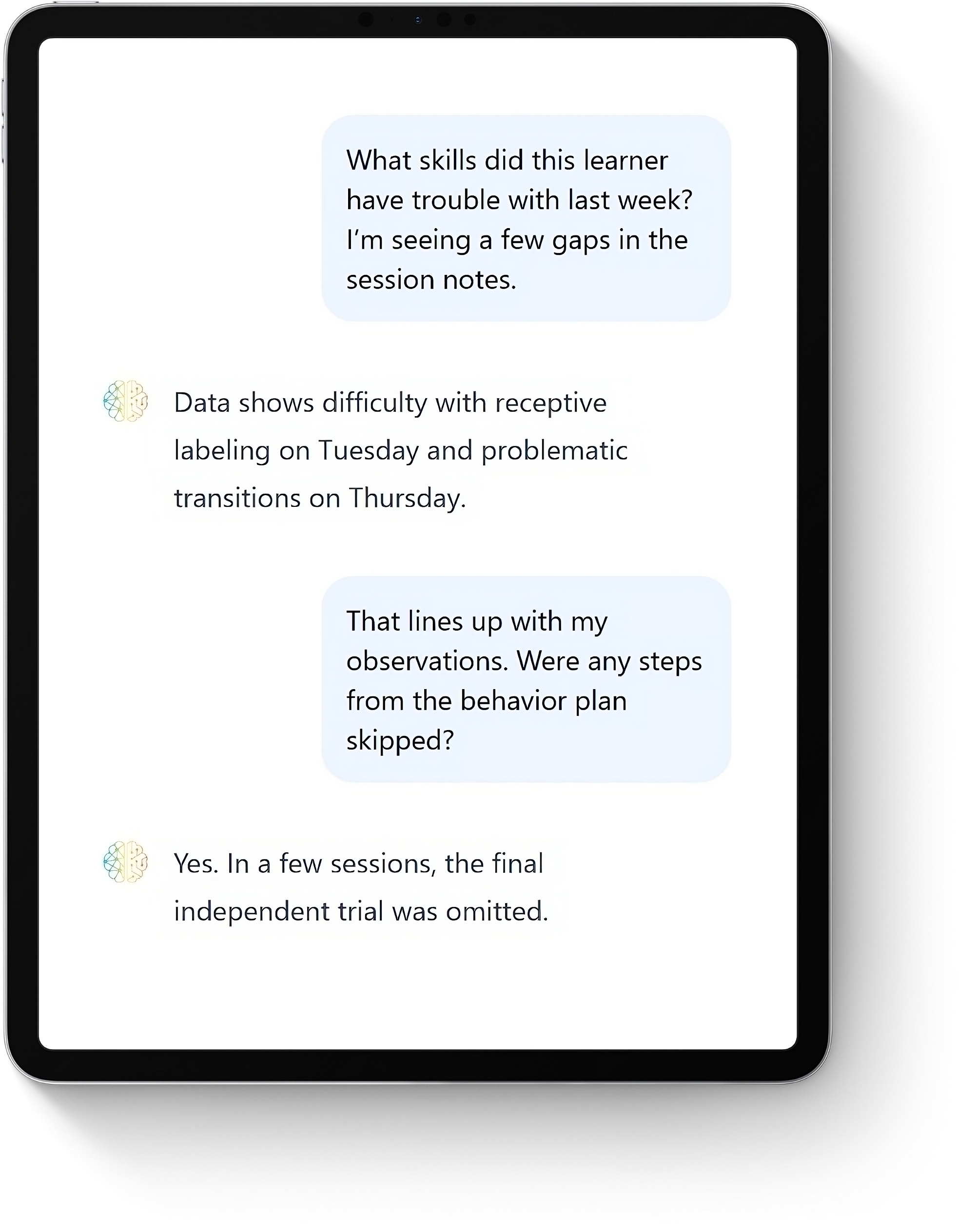
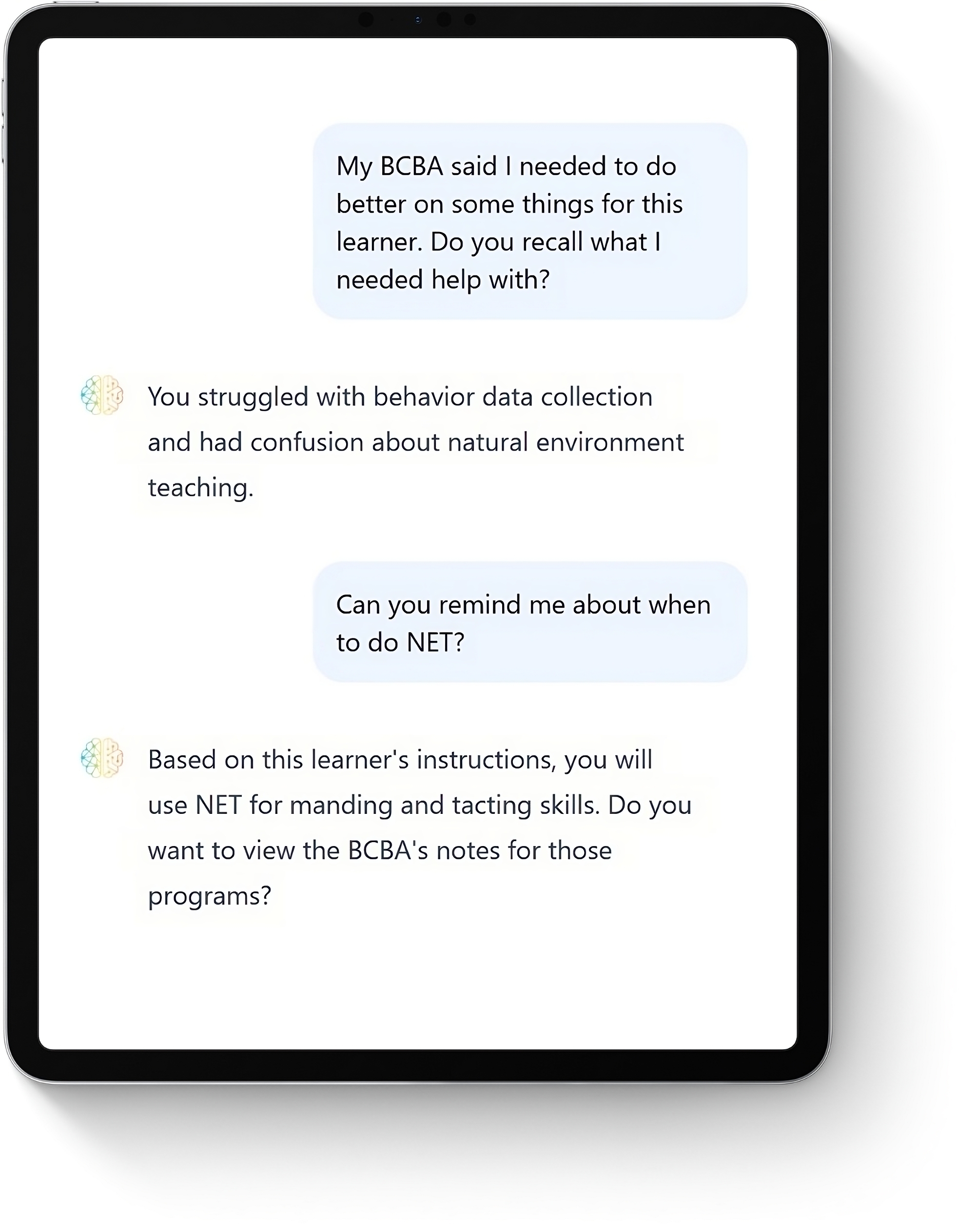
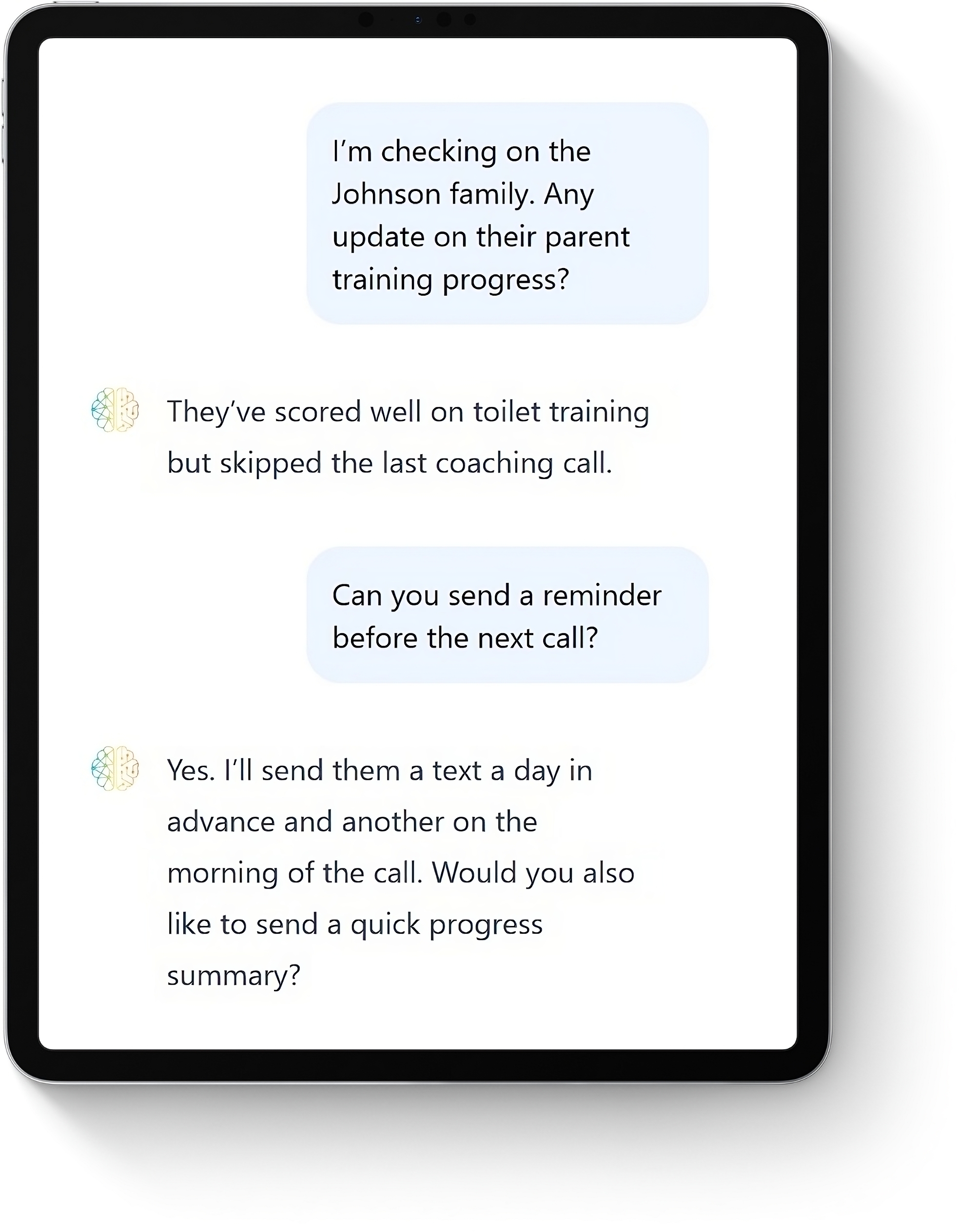
Our Conversational-AI Solution
"Show me Adrian's progress this month for all receptive language skills." Nia Chat reads relevant session data via EHR integration or data upload, then compiles an expert summary in seconds.